Abstract
Background: Inotuzumab-ozogamicin (IO) is one of the drugs of choice for relapse/refractory (R/R) acute lymphoblastic leukemia (ALL). Patients who received IO in a clinical trial had a CR rate of approximately 81% and a median overall survival of approximately 8 months, superior to best available therapy and numerically comparable with blinatumomab. Toxicities were generally manageable, veno-occlusive disease/ sinusoidal obstruction syndrome (VOD/SOS) was reported as a rare adverse event possibly linked to the drug that require attention, especially during hematopoietic stem cell transplant after IO. Data on IO effectiveness in the real-life setting are generally lacking, for the low incidence of the disease and the high number of possible therapies that are emerging.
Methods: INO-CD22 (NCT03898128) is a real-life study collecting data on safety, effectiveness and indirect costs of IO therapy in R/R ALL. Twenty-four Italian institutions enrolled patients who received IO in the post-market expanded access program or with national health system reimbursement. This study was approved by the ethical committee (Prot.9296/2018). Here we present preliminary results of effectiveness and treatment emergent toxicity.
Results: From 2014, we collected data of 65 patients who received IO and were evaluable for effectiveness and toxicity. Median age at start of IO was 47 years (IQR 27-61), 35 patients (53.9%) were male, 14 (21.5%) had Ph+ ALL. 12 patients (18.5%) received IO after 1 previous line of therapy, 16 (24.6%) after 2 previous lines, and 37 (56.9%) after more than 2 lines. In our patient set, 37 (56.9%) patients received IO after blinatumomab failure and 24 (36.9%) after an allogenic HSCT. Nine patients (13.8%) received IO after an history of mild to moderate liver-related adverse events.
Median number of IO courses administered was 1 (IQR 1-2). Three patients do not complete course 1, as they died for infection (2) and cerebral hemorrhage (1). Of the 60 patients who were alive after a course of IO, 56 have evaluable data, 47 (83.9%) obtained a complete remission with IO. Particularly, CR was obtained in 9/11 (81.8%), 11/15 (73.3%), and 27/30 (90.0%) evaluable patients who received IO as a 1 st, 2 nd or >2 nd salvage, respectively. Twenty-four out of 30 (80.0%) evaluable patients who received IO after blinatumomab failure and 17/18 (94.5%) patients who already received an HSCT achieve CR with IO.
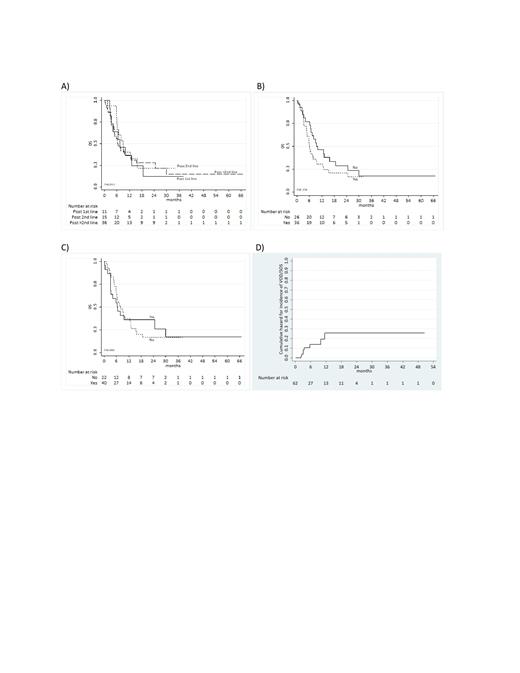
With a median follow-up of 25.7 months (95% C.I. 19.8-34.3), median OS was 7.5 months (95% C.I. 5.8-10.0). Median OS was 7.5 months (95% C.I. 2.7-18.6), 9.0 months (95% C.I. 5.8-15.8), and 6.4 months (95% C.I. 4.5-12.8) in patients who received one previous line of treatment, two lines of treatment, and more than two lines of treatment, respectively (figure A). Median PFS was 4.1 months (95% C.I. 0.1-13.21), 6.7 months (95% C.I. 0.1-12.4), and 5.0 months (95% C.I. 3.12-7.9) in patients who received one previous treatment line, two previous lines, and more than two lines, respectively.
Patients who received IO after blinatumomab failure had a median OS of 6.0 months (figure C, 95% C.I. 4.7-9.3). Patients who received IO after an HSCT had a median OS of 6.4 months (figure C, 95% C.I. 3.1-24.7). Twenty-five patient (38.5%) received an HSCT after IO therapy, of 22 (88.0 %) in CR, and 1 (6.7%) after further salvage therapies (chemotherapy).
During IO therapy, 1 treatment related toxic death and 1 treatment related VOD/SOS, 1 grade 5 infection (AE), 9 grade 3-4 AEs, and 25 grade 1-2 AEs were noted. The most common AEs during IO therapy were Thrombocytopenia (reported in 7 (10.8%) of patients), infections (reported in 6 (9.2%) of patients) and liver tox adverse events (reported in 6 (9.2%) of patients). Overall, 7 VOD-SOS were reported, and the incidence was higher during transplant.
Conclusions: Our data confirm in the real-life setting the great effectiveness of IO in term of CR. OS was comparable with data reported in clinical trials, even in a patient population that was not selected with inclusion criteria. OS and CR rate was not dramatically diminished in patients who already received HSCT nor in patients who already received blinatumomab. Safety of IO treatment was confirmed. IO is an easy-to-administer and safe therapy with a very high rate of expected CR in all the contexts and that confer promising expectation of survival.
Papayannidis: Novartis: Honoraria; Pfizer: Honoraria; Amgen: Honoraria; AbbVie: Honoraria; Astellas: Honoraria; Janssen: Honoraria. Fracchiolla: Amgen: Honoraria, Membership on an entity's Board of Directors or advisory committees; Pfizer: Honoraria, Membership on an entity's Board of Directors or advisory committees; Jazz: Honoraria, Membership on an entity's Board of Directors or advisory committees; Gilead: Honoraria, Membership on an entity's Board of Directors or advisory committees; Abbvie: Honoraria, Membership on an entity's Board of Directors or advisory committees. Di Raimondo: Amgen: Honoraria; AbbVie: Honoraria; Pfizer: Honoraria; Jazz Pharmaceutical: Honoraria; Janssen Pharmaceuticals: Honoraria; Bristol Myers Squibb: Honoraria. Lanza: Pfizer: Research Funding; Abbvie: Consultancy; Jazz: Consultancy; Sanofi: Consultancy. Borlenghi: Amgen, Janssen: Consultancy. Sica: Pfizer: Honoraria. Corradini: AbbVie, ADC Theraputics, Amgen, Celgene, Daiichi Sankyo, Gilead/Kite, GSK, Incyte, Janssen, KyowaKirin, Nerviano Medical Science, Novartis, Roche, Sanofi, Takeda: Honoraria; AbbVie, ADC Theraputics, Amgen, Celgene, Daiichi Sankyo, Gilead/Kite, GSK, Incyte, Janssen, KyowaKirin, Nerviano Medical Science, Novartis, Roche, Sanofi, Takeda: Consultancy; KiowaKirin; Incyte; Daiichi Sankyo; Janssen; F. Hoffman-La Roche; Kite; Servier: Consultancy; Amgen; Takeda; AbbVie: Consultancy, Honoraria, Other: Travel and accommodations; Novartis; Gilead; Celgene: Consultancy, Other: Travel and accommodations; BMS: Other: Travel and accommodation; Sanofi: Consultancy, Honoraria; Incyte: Consultancy; Novartis, Janssen, Celgene, BMS, Takeda, Gilead/Kite, Amgen, AbbVie: Other: travel and accomodations. Luppi: Abbvie: Honoraria; Novartis: Honoraria; Sanofi: Honoraria; MSD: Honoraria; Gilead Science: Honoraria, Other: Travel grant; Daiichi-Sankyo: Honoraria; Jazz Pharma: Honoraria. Pane: Novartis Pharma SAS;: Research Funding; AbbVie; Amgen; Novartis: Other: Travel, accommodation, expenses; AbbVie; Amgen; Novartis, GSK, Incyte: Speakers Bureau; AbbVie; Amgen; Novartis, GSK , Incyte: Consultancy. Passamonti: Janssen: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; BMS: Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; AbbVie: Speakers Bureau; Celgene: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Novartis: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau. Martinelli: Stemline Therapeutics: Consultancy; Astellas: Consultancy, Speakers Bureau; Roche: Consultancy; Incyte: Consultancy; Celgene /BMS: Consultancy, Speakers Bureau; Abbvie: Consultancy; Pfizer: Consultancy, Speakers Bureau; Daichii Sankyo: Consultancy; Jazz Pharmaceuticals: Consultancy.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal